In the human body there are many different tissues holding your bones and joints together. One of the
strongest types of tissue holding your body together is called a ligament. Ligaments hold one bone to the
next bone, and there are a huge number of them around each and every one of your joints.
In your ankle there are many ligaments that each need to be tight and strong to keep your ankle
functioning properly. Each ligament has a name and some are known to be weaker than others. When
you have chronic ankle sprains caused by weak ankles, the most common ligament to cause trouble is
called the Anterior Talofibular Ligament (a.k.a. ATFL) and the second most common is the
Calcaneofibular Ligament (a.k.a. CFL). The ligaments can be stretched, inflamed, partially or completely
torn. There are multiple other ligaments around the outside of your ankle that hold the joint together and
keep the ankle strong.
Although the ATFL and CFL are the most commonly injured, any number of the nearby ligaments can
also be damaged.
When these ligaments are injured repeatedly and don’t heal properly they allow for the ankle joint to move
in ways that can lead to damage. The cartilage, bones, and soft tissue that makes up your ankle joint will
likely become inflamed with repeated injury, leading to stretching and eventual scarring around your
ankle.
Each of these things, ligament injury, cartilage injury, bone injury, and diffuse soft tissue injury can
contribute to chronic ankle sprains, weak ankles and ankle pain. Each of them is addressed in a different
way, and Dr. Pathak Founder and CEO of Pathak Podiatry P.C. has more than 10 years of experience at
determining what surgery you need to correct each individual component of your pain.
If you’ve already failed conservative treatment that means the tissues around your ankle may be too
weak, torn, or scarred to hold your ankle in place. Without surgery these tissues may never repair
themselves and you will continue to have ankle sprains and experience pain.
Loose ligaments and soft tissues can allow for improper wear on your joints over time. Fixing the chronic
ankle instability with a soft tissue procedure is easier to heal and less painful in the long run than trying to
correct years of injury to the joints.
If you choose not to have surgery, your chronically weak ankle(s) can be braced using firm shoe gear or
custom made foot orthotics and strengthened with ankle exercises. If you choose not to have the surgery and you don’t support your ankle in some way, you will continue to
sprain your ankle and you may even eventually end up breaking your ankle. There is a possibility that you
could damage the cartilage and joints in your ankle joint which is very difficult to heal once damaged.
A good candidate for ankle stabilization is someone who has tried conservative treatment for several
months, including strengthening exercises, custom orthotics and shoe modification with no relief. This
includes individuals who suffer from repeated ankle sprains, making daily activities difficult, and
individuals who tend to roll their ankles frequently due to having weak ligaments.
While there are several variations to an ankle stabilization procedure. Choosing between procedures is
based on what structures are weak in your ankle, the severity of the injury, and your surgeon’s
preference. Deciding which procedure to perform requires a physical exam from a skilled doctor and
possibly additional imaging studies like an MRI. The most common procedure is called a Brostrom
procedure and it includes several key steps listed below.
● In the lateral ankle stabilization surgery the first thing your surgeon will do is position your foot so
that they have the best possible view of the outside of your ankle. Then they will make a cut in the
skin and dissect down to the damaged ligaments. The size of the cut can vary depending on
which combination of procedures you personally need performed.
● The doctor will inspect your ligaments for tears, scarring and thinning. If the ligament is intact it
will be cut, and tightened by sewing it back together in a new shorter and stronger position. If the
ligament is already ruptured it will be cleaned, and sewn together in the stronger shorter position.
○ Two ligaments in the ankle can be addressed this way, one is the ATFL discussed above,
and the second is the Calcaneofibular Ligament (a.k.a. CFL). Both can be repaired,
however, both do not always need repair. Certain tests before your surgery can help
determine which, if not both, need repair.
● Your doctor may use strong thread/suture attached to small metal bone anchors to strengthen
your ligaments even more by reinforcing them. The bone anchors may be made of metal, or
multiple other materials. The purpose of the thread and anchors is to brace your own ligaments
while they heal, and provide stability. The two anchors will be placed into your bone, and the
strong thread will be tightened between the two anchors over top of the repaired ligaments. This
is a very popular technique used by surgeons to strengthen the outside of your ankle.
● Once the ligaments are tightened and reinforced the tissue around the outside of your ankle is
sewn back together carefully to bring additional stability to the repair. The skin incision is closed
with stitches and a bandage is placed over the top.
● You will have a custom made splint around your ankle for the first week after surgery, possibly
longer. The splint will prevent you from moving your ankle, which allows the stitches to heal.
In the rare circumstance that you have a severely weak ankle with little to no ligament left to repair, we
may consider doing a more advanced procedure.
This procedure involves taking a graft tendon, and using it to reconstruct your ATFL and CFL ligaments.
This procedure is significantly more complicated than the Brostrom procedure described above. An
additional incision behind your ankle bone on the outside of your ankle will be required. The additional
incision may be straight, or curved and can be 3-5cm long. The tendon graft is anchored in 2 places, one
anchor in the calcaneus (heel bone) and one in the talus. Your surgeon skillfully recreates the ATFL and
CFL ligaments using the tendon graft, tightening each newly constructed ligament independently to
support your ankle.
In some cases it will be necessary to move your heel bone over to limit the inward position of your heel. If
this more advanced procedure is necessary, your doctor will discuss exactly what they plan to do before
the surgery. Every person is different, and your procedure may not follow exactly the protocol listed
above.
There are several common risks with surgery. In addition to these general risks, there are a few specific
risks associated with the ankle stabilization surgery that you should be aware of.
First and foremost, the risk of needing a second surgery with an ankle stabilization procedure is higher
than some other common foot surgeries. This is because your ligaments, while sewn together in a tighter
position during the surgery, have the potential to loosen again over time. We do everything possible to
avoid these potential complications by providing you with the knowledge and material to recover
completely before returning to activity.
Second, there is a minor risk of over-tightening the ligaments of the ankle. You may feel like your ankle is
unusually tight after ankle stabilization surgery, this is normal and may require some adjusting.
There is a risk of injury to a specific nerve that runs down the top of your foot near the surgical site. This
nerve provides feeling to part of the top of your foot, and if damaged may result in loss of sensation to
part of the top of your foot.
The best way to avoid complications is to follow your doctor’s orders carefully after surgery, and report
any sudden or painful changes in your ankle. Picking a skilled surgeon with extensive experience in
sports medicine and ankle stabilization always helps reduce your risk of complications.
The main goal of a successful ankle stabilization surgery is to reduce pain from chronic sprained ankles
and possible future arthritis or injury. Ankle stabilization surgery with appropriate rehabilitation can allow
you to return to your favorite shoe gear and activities. Everyone’s surgical experience is different, and
your recovery and results may vary. We have many years of experience producing good results with safe
recoveries.
With the correct surgeon and post operative physical therapy, many individuals return to walking, running
and even sports activities after the ankle stabilization surgery.
You will be fully non-weight bearing for 2-4 weeks. That means you will not be able to walk, or stand
without either crutches or a knee scooter. At 2-4 weeks after surgey you can start transitioning to weight
bearing. This involves gradually placing increasing amounts of your body weight on the ankle. By 6 weeks
you will likely be fully weight bearing and able to walk. All surgical results vary, and it can take longer to
recover for some individuals.
If we operate on the right foot, you will not be able to drive for several weeks. You will be wearing a
surgical boot for 4-6 weeks after the surgery, which prevents you from driving. If we operate on the left
ankle you may be able to drive much sooner, because the surgical boot will not be in the way of an
automatic car’s pedals. We advise patients to avoid driving until you feel you can safely make an
emergency stop.
With the proper physical therapy many athletic patients are able to slowly return to activity at the 12 week
mark after surgery. If the surgery is more complex and involves additional bone anchors and tendon
grafts, this may be significantly longer.
While most people begin to return to activity at 8 weeks, it can take up to a year to retrain the ankle and
fully return to normal after an ankle stabilization procedure. Close adherence to your surgeon’s recovery
plan and attending physical therapy are key for the most speedy recovery.
The Brostrom ankle stabilization surgery is a very good and reliable surgery for stabilizing a chronically
weak ankle. A study published in 2017 looked at the outcomes of 669 Brostrom procedures and found the
need for a second operation was only 1.2% on average 8.4 years after their Brostrom procedures. Now,
it’s important to note that each ankle is different, and your ankle may be more severely injured than
others, making a reoperation more likely.
In the circumstance you have an unstable CF ligament or you do need a second operation, we would
likely move on to the tendon graft procedure described above.
If you’ve met with an experienced foot and ankle surgeon, and decided together that it’s time to pursue
surgery, the next step is preparing for that surgery.
Dr. Pathak and her staff will guide you through the preoperative process, details of the operation and post
operative recovery.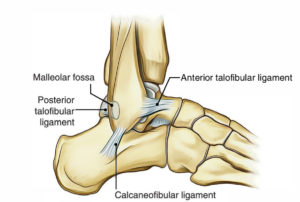
Dr. Neha Pathak brings extensive experience to her role as a podiatrist at Pathak Podiatry.
Managed & Designed by – Alltic Healthcare